

Click one of the links below for more information about:
Diseases We Commonly Treat:
Common Reasons for Referral to a Gastroenterologist
Disclaimer: All information contained on this website is intended for informational and educational purposes. The information is not intended nor suited to be a replacement or substitute for professional medical treatment or for professional medical advice relative to a specific medical question or condition. We urge you to always seek the advice of your physician or medical professional with respect to your medical condition or questions. As a recipient of information from this website, you are not establishing a doctor/patient relationship with any physician. There is no replacement for personal medical treatment and advice from your personal physician.
Diseases We Commonly Treat
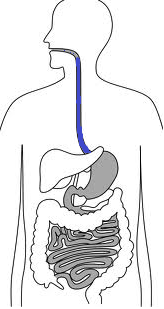
Esophagus
BARRETT’S ESOPHAGUS
- A condition, usually caused by uncontrolled GERD, where the lining of the esophagus becomes precancerous.
- Canadian guidelines recommend that patients who have had reflux symptoms for more than 10 years undergo a one-time GASTROSCOPY to screen for Barrett’s Esophagus.
ESOPHAGEAL CANCER
- The most common cause is smoking. Other causes include longstanding uncontrolled GERD, alcoholism, or family history of esophageal cancer.
- Canadian guidelines recommend that patients who have had reflux symptoms for more than 10 years undergo a one-time GASTROSCOPY to screen for BARRETT’S ESOPHAGUS.
ESOPHAGEAL MOTILITY DISORDERS
- A group of conditions where the normal muscle movement of the esophagus becomes uncoordinated. It usually causes symptoms such as difficulty swallowing both liquid and solid food.
- It is diagnosed by GASTROSCOPY as well as other specialized tests for the esophagus.
- It can be caused by GERD, medications, and other health problems such as diabetes.
- There are a variety of prescription medications that can be used for this condition.
ESOPHAGITIS
- Inflammation in the lining of the esophagus. The most common cause is GERD. Other causes include smoking, medications and other health problems. It is diagnosed by GASTROSCOPY, and treated with prescription medications.
GASTROESOPHAGEAL REFLUX DISEASE (GERD), also called Acid Reflux Disease.
- A condition where the acid contents of the stomach move into the esophagus.
- Possible symptoms include: heartburn, reflux (food coming back up), indigestion, cough, worsening asthma, or swallowing difficulties.
- Can sometimes lead to damage occurring in the esophagus, although not always.
- Can lead to ESOPHAGITIS (inflammation of the esophagus), PEPTIC STRICTURES (narrowing of the esophagus), BARRETT’S ESOPHAGUS (precancerous changes in the lining of the esophagus), or ESOPHAGEAL CANCER.
- Most common cause is weight gain. Other causes include certain foods, smoking, side effects of medications or other health problems. Stress can often worsen symptoms.
- The most effective way to treat is weight loss. Stop smoking is important. Avoiding certain foods can also be helpful, such as chocolates, caffeine, red wine, spicy food, and acidic foods such as oranges and tomatoes. It is important to wait at least 30 to 45 minutes after eating before lying down. If symptoms occur at night, then raising the head of the bed by at least 15 degrees may be helpful.
- There is a long list of medications that can be helpful. Some are prescription and some are over-the-counter. You should consult with a doctor or pharmacist before starting these medications.
HIATUS HERNIA
- A condition where part of the stomach slides above the diaphragm. It is often associated with GERD, and presents with similar symptoms, mainly heartburn, reflux, indigestion or swallowing difficulties. The cause is unknown.
- It is diagnosed by specialized xray studies or by GASTROSCOPY..
- Effective treatments are similar to those used for GERD. Please see above.
PEPTIC STRICTURES
- A condition where part of the esophagus becomes narrowed. It can cause difficulty swallowing.
- It is usually caused by GERD. Other causes include smoking, medications and other health problems.
- It is diagnosed by specialized xray studies or by GASTROSCOPY.
- A stricture can be dilated during GASTROSCOPY. Medications are used to prevent recurrence.
SCHATZKI’S RING
- A narrowing at the bottom of the esophagus. The most common symptom is solid food occasionally getting stuck while eating.
- It is not cancerous.
- It is diagnosed by GASTROSCOPY. It is treated by being dilated at the time of GASTROSCOPY.
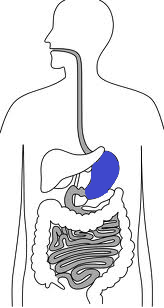
Stomach
EROSIONS
- A small area where the lining of the stomach erodes away.
- If it becomes larger it turns into an ulcer.
- It can cause symptoms such as stomach pain, heartburn or indigestion.
- It can be caused by medications, especially Aspirin or anti-inflammatory medications such as Advil or Ibuprofen. It can also be caused by bacteria called H PYLORI, by smoking, or by other health problems.
- It is diagnosed by GASTROSCOPY.
- It is treated with prescription medications.
GASTRIC CANCER
- The most common causes are smoking and alcoholism. People of Asian background are at higher risk, and those with a family history of gastric cancer. H PYLORI, a bacteria, can sometimes cause a rare type of gastric cancer.
- There are no guidelines for routine screening of gastric cancer.
GASTRITIS
- Inflammation of the lining of the stomach. The most common causes are alcohol, bacteria called H PYLORI, or medications, especially Aspirin or anti-inflammatory medications such as Advil or Ibuprofen. Very spicy foods can also be irritating to the lining of the stomach.
- It is diagnosed by GASTROSCOPY, and treated with prescription medications.
GASTROPARESIS, also called Delayed Gastric Emptying
- A condition where the stomach takes a very long time to move the food contents into the small bowel. It can cause symptoms such as nausea, vomiting and reflux.
- It is most commonly caused by medications, and other health problems, such as diabetes.
- It is diagnosed by GASTROSCOPY or specialized stomach x-rays.
- It is treated with a variety of prescription medications.
GASTRIC ULCERS
- An ulcer is an area where the lining of the stomach erodes away. It can cause symptoms such as heartburn, abdominal discomfort, nausea, vomiting, indigestion or bleeding.
- It can be caused by medications, especially Aspirin or anti-inflammatory medications such as Advil or Ibuprofen. It can also be caused by bacteria called H PYLORI, by smoking, or by concurrent medical conditions.
- It is diagnosed by GASTROSCOPY.
- It is treated with prescription medications.
HELICOBACTER PYLORI
- A bacteria that lives in the lining of the stomach. It is very common, and is acquired by ingesting it with your food.
- It does not cause any symptoms in the majority of people. It can sometimes cause abdominal discomfort or heartburn.
- It has been associated with GASTRIC ULCERS, DUODENAL ULCERS, and very rarely an unusual type of GASTRIC CANCER.
- It can be diagnosed by blood test, a specialized breath test, or by GASTROSCOPY.
- It is treated with antibiotics.
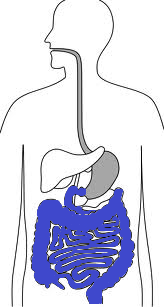
Small and Large Intestines
CELIAC DISEASE (SPRUE)
- A condition where the lining of the small bowel (duodenum) erodes in reaction to eating Gluten, a food ingredient found in wheat, rye, barley and sometimes oats.
- It can present with a variety of symptoms, including abdominal bloating, diarrhea, weight loss, low iron or low blood counts (anemia), rash, or thinning of the bones (osteoporosis).
- It is diagnosed with blood tests and a GASTROSCOPY
- It is treated by eliminating all sources of gluten from the diet. It is a lifelong condition.
- See GLUTEN INTOLERANCE as well
CLOSTRIDIUM DIFFICILE
- A bacteria usually acquired in the hospital, that causes severe diarrhea.
- It is diagnosed with stool tests or by colonoscopy.
- It is treated with antibiotics.
- The majority of cases are cured with antibiotics, but it can be very difficult to treat. In elderly and sick patients, it can be very serious and potentially cause death.
- It is spread very easily in hospitals, and is prevented with proper hand washing by all hospital staff and visitors.
COLON CANCER SCREENING
- Colon cancer is one of the only cancers that we can detect and remove before it turns into a cancer, thereby completely preventing it.
- Canada has one of the highest rates of colon cancer. It is the third most common cancer after breast and lung. It occurs in men and women equally. The lifetime risk is 6% without a family history.
- Screening is recommended for everyone over the age of 50.
- Screening may be recommended earlier for those with a family history of colon cancer.
- There are a variety of screening options, and these should be discussed with your family physician or gastroenterologist.
CROHN’S DISEASE
- A condition where patches in the lining of the bowel erode away.
- Can occur anywhere in the bowel from the mouth to the rectum, but the most common locations are at the end of the small bowel, called the terminal ileum, and the large bowel, called the colon.
- The cause is still not fully understood, but a family history of INFLAMMATORY BOWEL DISEASE is considered a risk factor.
- Can present with a variety of symptoms, including fever, weight loss, abdominal pain, diarrhea or rectal bleeding.
- It is diagnosed with COLONOSCOPY and /or bowel x-rays.
- It is treated with a variety of prescription medications. There is no cure, but with current treatment it is possible to achieve remission, meaning the disease is not active, for prolonged periods of time. There is no scientific evidence that naturopathic remedies are effective for this disease.
DIVERTICULAR DISEASE
- Diverticulosis is a condition where small out-pouches or pockets occur in the lining of the large bowel (colon).
- It is very common in North America, occurring in up to 50% of people at the age of 50 years old.
- The cause is unknown, but it is thought to be associated with inadequate fibre in the diet.
- The majority of the time it does not cause any symptoms. Occasionally it can be associated with lower abdominal discomfort. This often occurs in the setting of constipation.
- Sometimes this condition can lead to inflammation of one of the out-pouches, called diverticulitis. This is associated with severe pain and fever.
DUODENAL ULCERS
- An ulcer is an area where the lining of the bowel erodes away. In a duodenal ulcer it occurs in the duodenum, the start of the small bowel just beyond the stomach. It can cause symptoms such as heartburn, abdominal discomfort, nausea, vomiting, indigestion or bleeding.
- It can be caused by medications, especially Aspirin or anti-inflammatory medications such as Advil or Ibuprofen. It can also be caused by bacteria called H PYLORI, by smoking, or by concurrent medical conditions.
- It is diagnosed by GASTROSCOPY.
- It is treated with prescription medications.
GLUTEN INTOLERANCE
- A condition where eating gluten causes abdominal bloating, diarrhea, fatigue or feeling generally unwell.
- Unlike CELIAC DISEASE, in patients with gluten intolerance all of the tests for celiac disease are negative.
- Unlike CELIAC DISEASE, gluten intolerance is often NOT a life-long condition, but rather can come and go intermittently.
- The cause of gluten intolerance is not known.
- The only treatment for gluten intolerance is to eliminate gluten from the diet until symptoms improve.
INFLAMMATORY BOWEL DISEASE
- A category of diseases that cause inflammation in the bowel. The most common types are CROHN’S DISEASE and ULCERATIVE COLITIS.
IRRITABLE BOWEL SYNDROME
- A condition that causes abdominal bloating or discomfort, usually but not always associated with a change in bowel habits, either diarrhea or constipation.
- The cause is not known. It is commonly associated with stress or anxiety. It can often be triggered by an infection or episode of food poisoning, but the symptoms persist long after the infection or poison has left the body.
- It is diagnosed mostly based on symptoms. The gastroenterologist may perform tests to exclude other diseases as well as to provide reassurance that everything is normal on examination.
- Treatment consists of reassurance, supplements or medications to make the bowels more regular, and stress management. There is evidence that Probiotics, supplements containing a mixture of bacteria that normally exist in the bowel, may be helpful for this condition as well.
- There is no cure, but the symptoms can resolve spontaneously for a period of time or forever.
LACTOSE INTOLERANCE
- We are all lactose intolerant to various extents. We continue to gradually lose our ability to digest lactose as we age. When we are eating more lactose than we can digest, we develop symptoms of lactose intolerance.
- Symptoms include excess gas, bloating, abdominal cramps and diarrhea.
- There is no one test that is particularly good at diagnosing lactose intolerance. The best way to confirm lactose intolerance is to avoid all food and beverages containing lactose for two weeks – if you feel better, then you are lactose intolerant.
- Treatment is decreasing the amount of lactose you are currently consuming. You can also try over-the-counter Lactaid pills, which are helpful for some people, but not everyone.
ULCERATIVE COLITIS
- A condition where the lining of the large bowel, also called the colon, erodes away.
- The cause is still not fully understood, but a family history of INFLAMMATORY BOWEL DISEASE is considered a risk factor.
- Symptoms can include abdominal pain, fever, weight loss, diarrhea or rectal bleeding.
- It is diagnosed with colonoscopy.
- It is treated with a variety of prescription medications. The only cure is removal of the colon, which is very rarely done, and only in extreme circumstances. With current treatment it is possible to achieve remission, meaning the disease is not active, for prolonged periods of time. There is no scientific evidence that naturopathic remedies are effective for this disease.
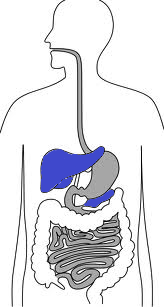
Liver, Gallbladder, and Pancreas
ALCOHOLIC LIVER DISEASE
- Excessive alcohol use can lead to permanent liver damage, liver failure and death. The amount of alcohol needed to cause damage is different in every person.
- It is recommended to have less than 7 drinks per week for women, and less than 14 drinks per week for men. It is also recommended that on any one occasion, to have less than 3 drinks for women, and less than 4 drinks for men.
FATTY LIVER DISEASE
- Caused by too much fat in the liver. It is the most common cause of abnormal liver tests in North America today.
- In some people does not cause any damage to the liver. In others, can cause liver scarring, permanent damage (called cirrhosis), liver failure or death. It is impossible to predict who will progress to liver damage.
- The only effective treatment currently is weight loss and exercise.
GALLSTONES
- Are small stones that appear in the gallbladder. It normally occurs in up to 50% of the population.
- The cause is not clearly understood.
- A gallstone normally passes from the gallbladder to the bowel along a tube called a bile duct. A gallstone attack occurs when the stone is too big and gets stuck in the bile duct.
- Symptoms include severe abdominal pain in the right upper quadrant, often radiating around to the back. It can be associated with fever, turning yellow (jaundice), pale stools or dark urine.
- The stone sometimes eventually passes on its own. Otherwise treatment involves a procedure called ERCP (endoscopic retrograde cholangiopancreatography), where a tube is placed through the mouth into the small bowel and up the bile duct, and the stone is removed.
- Once a gallstone attack occurs, it is very likely that it will happen again, and thus the recommended treatment is removal of the gallbladder (cholecystectomy), soon after you have recovered from the attack.
HEMOCHROMATOSIS
- A condition where the body accumulates too much iron, which starts to deposit in the liver, as well as other organs.
- It is a genetic condition inherited from your parents.
- It is diagnosed on blood tests and liver biopsy (examining a microscopic sample of the liver obtained with a needle).
- It is treated by removing iron from the body at regular intervals, usually by removing small amounts of blood.
- It can cause permanent liver damage (cirrhosis) and liver failure, although this is very rare today in North America because family doctors usually detect it very early as part of their investigations done on routine check-ups.
HEPATITIS A
- A virus that you can get from eating improperly cleaned foods.
- Causes sudden onset right upper quadrant abdominal discomfort, fever, turning yellow (jaundice), general aches, vomiting or diarrhea.
- 95% of the time it resolves on its own.
- There is a vaccine available that prevents you from getting Hepatitis A. You can ask your family physician to give you the vaccine.
HEPATITIS B
- A virus that you can get from sexual intercourse. You can also get it from improperly sterilized needles (illicit drug use or possibly tattoos). It is very rare to get it today from a blood transfusion in Canada. It is possible to get the virus at birth if the mother is infected. It is possible to get the virus as a child if you are raised in a country where it is very common, or grow up in a household with other people that are infected.
- The majority of people that get Hepatitis B as a child end up keeping the virus in their body (chronic infection).
- Most of the time chronic Hepatitis B does not cause any symptoms. Rarely it can cause abdominal discomfort, turning yellow (jaundice), fever or loss of appetite.
- The virus behaves differently in every person. In some people it never causes liver damage. In others, it can cause permanent liver damage, called cirrhosis, liver cancer, liver failure or death.
- There is no cure. Antiviral drugs are used to keep the virus from causing damage to the liver. We decide to use these drugs depending on how the virus is behaving in your body. It is different for every patient.
- Vaccines are available to prevent you from getting Hepatitis B. You can ask your family physician to give you the vaccine.
HEPATITIS C
- A virus that you can get from improperly sterilized needles (illicit drug use or possibly tattoos). It is very rare to get it today from a blood transfusion in Canada.
- The majority of people that get Hepatitis C as an adult end up keeping the virus in their body (chronic infection).
- Most of the time chronic Hepatitis B does not cause any symptoms. Rarely it can cause abdominal discomfort, turning yellow (jaundice), fever or loss of appetite.
- The virus behaves differently in every person. In some people it never causes liver damage. In others, it can cause permanent liver damage, called cirrhosis, liver cancer, liver failure or death.
- There is a cure for the majority of people with a combination of antiviral drugs. The treatment, however, is not guaranteed to work, but can be effective in up to 80% of patients, depending on the type of Hepatitis C infection, and the amount of damage that has been caused to the liver.
- There is no vaccine available for Hepatitis C.
PANCREATITIS
- A condition where the pancreas becomes inflamed.
- The most common causes are gallstones and excessive alcohol use.
- The symptoms usually are severe abdominal pain, often associated with nausea and vomiting, and occasionally fever.
- The treatment usually involves treating the underlying cause, such as to stop drinking, or removal of the gallstone.
Common Reasons for Referral to a Gastroenterologist
- Anemia or Low Blood Count
- Bad Breath
- Bleeding – from the mouth or rectum
- Bloating
- Burping
- Change in bowel habits or shape of stool
- Colon Cancer Screening
- Constipation
- Diarrhea
- Gallstones
- Gas
- Heartburn
- Hemorrhoids
- Incontinence – unable to control bowel movements
- Indigestion
- Liver Disease
- Nausea
- Pain or discomfort – in throat, chest, abdomen, rectum or anus
- Swallowing Difficulties
- Vomiting
- Weight loss
Follow us on